What Is ESI? Epidural Steroid Injection (ESI) is a treatment designed to relieve inflammation in the epidural space of your spine—the area that surrounds your spinal cord and nerve roots. The procedure involves injecting a corticosteroid (anti-inflammatory medication) along with a local anesthetic to reduce pressure and pain, usually caused by herniated discs, spinal stenosis, or degenerative disc disease.
The procedure doesn’t fix the structural issue permanently but gives your body time to heal by decreasing inflammation.
There are three main types of ESI in medical practice:
- Interlaminar Epidural Steroid Injection
- Caudal ESI
- Transforaminal ESI
We’ll explain each of these below.
ESI Medical Abbreviation: What Does ESI Stand For?
“ESI” stands for Epidural Steroid Injection—a therapeutic process used widely in pain management, especially for spinal and nerve-related pain conditions.
In clinical notes, you’ll often see “ESI L4-L5” or “Caudal ESI done” — abbreviations used to document the injection’s location and technique.
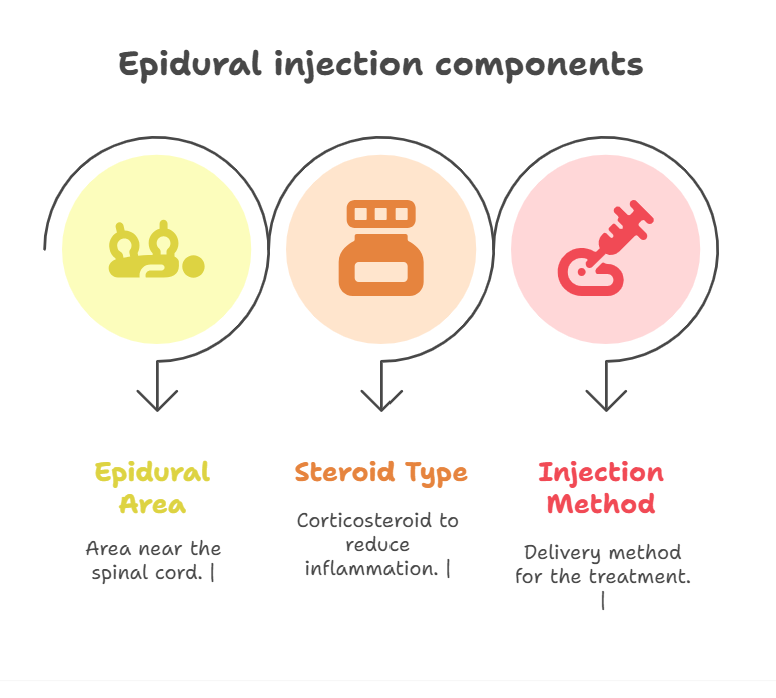
For patients, it’s helpful to know the lingo when reading discharge notes or appointments:
- Epidural = area near your spinal cord
- Steroid = corticosteroid, not muscle-building kind, used to reduce inflammation
- Injection = the delivery method for treatment
Types of Epidural Steroid Injections: Breaking It Down
Interlaminar Epidural Steroid Injection (Traditional Approach)
This is one of the most commonly used approaches. An interlaminar ESI is delivered between the laminae (bones of your spine), directly into the epidural space. It’s similar to the spinal anesthesia pregnant women might receive before delivery.
Best for: General back pain not isolated to a single nerve root.
Caudal ESI
This type of ESI is done through the sacral hiatus, an opening near the base of your spine. It’s less risky compared to other techniques and is usually ideal when multiple nerve roots may be involved.
Best for: Lower back pain, especially when stenosis is widespread or prior surgeries limit other routes.
Transforaminal ESI
Highly specific, this type is administered near nerve exits (foramina), allowing targeted delivery to a single inflamed nerve root. It’s often selected when MRI or CT pinpoints a single problem area—like sciatica or a herniated disc pressing on a nerve.
Best for: Targeted leg pain or sciatica.
Patient Experience: Real Voices on ESI Relief
One chronic pain sufferer shared their experience on a forum:
“I tried physical therapy and meds for 8 months with no relief. My caudal ESI gave me 70% relief in just three days. I wish I’d considered it earlier.”
While individual results may vary, stories like these show how effective ESIs can be when used correctly and at the right time in your treatment journey.
Common Conditions Treated by ESI
- Herniated or bulging discs
- Spinal stenosis
- Sciatica
- Degenerative disc disease
- Spondylolisthesis
- Post-laminectomy (failed back surgery) syndrome
These conditions often cause nerve inflammation, pain radiating to limbs, or tingling and weakness. ESI directly addresses the inflammation pressing on those nerves.
Best Position to Sleep After Epidural Steroid Injection
Pain after the procedure is normal, and sleeping position can make a difference. But what’s the best position to sleep after epidural steroid injection?
Here’s what most specialists recommend:
- Side-sleeping with a pillow between knees: This helps keep the spine aligned and avoids extra pressure.
- Back-sleeping with a pillow under knees: Keeps the lower back gently curved and can reduce strain.
Avoid:
- Sleeping on your stomach—this can arch your back and worsen inflammation.
Some also find a slight incline (in a recliner or elevated bed) helpful during the first 24–48 hours.
What to Expect Before, During, and After ESI
Before:
- You’ll likely undergo imaging (MRI, CT) to confirm the problem area.
- Avoid blood-thinners or NSAIDs a few days before.
- No food 4–6 hours beforehand.
During:
- Procedure lasts about 15–30 minutes.
- You may be mildly sedated.
- Guided via fluoroscopy (live X-ray) for precision.
After:
- Temporary soreness is normal.
- Maximum benefit typically kicks in 48–72 hours later.
- Relief can last several weeks to several months, depending on your condition.
Risks and Side Effects of ESI
Like all procedures, ESI has some risks—though complications are rare.
Possible side effects:
- Temporary headache
- Injection site pain
- Nausea
- Dizziness
- Elevated blood sugar (especially in diabetics)
- Rare nerve damage or infection
It’s crucial to share all health conditions with your doctor before undergoing ESI—especially if you’re on medications, have bleeding risks, or are pregnant.
ESI Alternatives: Is It Your Only Option?
If you’re not ready for an ESI or it didn’t help, know that you have options:
- Physical therapy
- Oral anti-inflammatory drugs
- Nerve ablation (burning nerve endings for longer relief)
- Surgery (if structural damage is severe)
- Acupuncture or chiropractic care (case-dependent)
But for many patients, ESI bridges the gap—delaying or even avoiding invasive surgery altogether.
FAQs
Q What does ESI stand for in medical terms?
A. In medicine, “ESI” means Epidural Steroid Injection, a procedure that delivers anti-inflammatory medication directly into the epidural space around your spinal cord to relieve nerve-related pain.
Q How long does it take for ESI to work?
A. In most cases, patients report improvement within 2–5 days after the injection. However, some feel relief within hours, while for others it may take up to a week.
Q How long does ESI pain relief last?
A. Relief duration varies from a few weeks to several months, depending on the severity of your condition, activity levels, and personal healing response. Repeat injections are often spaced at 3–6 month intervals if needed.
Q Is caudal ESI better than interlaminar?
A. Not necessarily. Caudal ESI is less invasive and safer for post-surgery patients, while interlaminar ESI delivers medication closer to the target area. The “better” method depends entirely on the patient’s anatomy and diagnosis.
Final Thoughts
When it comes to managing persistent nerve or spine pain, ESI isn’t a silver bullet—but it’s one of the most effective tools doctors use to give people their lives back.From the varying techniques like interlaminar epidural steroid injection and caudal ESI, to post-injection care like finding the best position to sleep, the success of this approach lies in understanding your specific condition and staying active in your recovery process.
CLICK HERE FOR MORE BLOG POSTS
“In a world of instant takes and AI-generated noise, John Authers writes like a human. His words carry weight—not just from knowledge, but from care. Readers don’t come to him for headlines; they come for meaning. He doesn’t just explain what happened—he helps you understand why it matters. That’s what sets him apart.”

